How To Fix Full Body Posture
Similar to other structures in the body, the cervical spine (CS) has a significant influence on body regions located above and below its location. Not only does CS musculature produce movement of the head and neck, but it also plays a key role in postural orientation reflexes, proprioceptive systems, vestibular function, and facilitating stabilization of the entire body. Similarly, in addition to localized dysfunction in the CS, sustained forward head posture (FHP) can bring about impairments in other body regions as well. Let's explore this subject more in depth below and how it relates to corrective exercise as a discipline! Forward head posture (FHP) - also known as Nerd Neck or Tech Neck - is an abnormality that can be identified by examining the position of their head with respect to the cervical spine (CS). Interestingly in FHP, not only does the head project anteriorly over the CS, but simultaneous tilting of the head in a posterior direction also occurs promoting hyperextension of the upper CS (Patwardhan et al., 2018). The backward rotation of the head on the CS is a compensation that enables an individual with FHP to look straight ahead instead of towards the ground (Patwardhan et al., 2018). If FHP becomes chronic, it can place large stresses on the muscles and connective tissue in the CS region (Patwardhan et al., 2018). As with other postural and movement dysfunctions throughout the body, FHP often results in movement compensations due to regional musculature becoming excessively underactive or overactive. The muscles that tend to become underactive in individuals with FHP include the deep neck flexors, cervical erector spinae, lower trapezius, and rhomboids (Clark et al., 2014). Underactivity in these muscles contribute to the inability to maintain an upright position of the CS. Muscles that often become overactive in those with FHP include the upper trapezius, levator scapula, scalenes, sternocleidomastoid, and suboccipitals (Clark et al., 2014). Overactivity of these muscles facilitate forward head migration, as well as in some cases, rounding of the shoulders. Read More: 12 Great Corrective Exercises for the Upper Back Advanced stages of FHP can contribute to upper CS compression which significantly reduces the ability of the first cervical vertebrae (C1) to rotate around the second vertebrae (C2) as it normally would (Pop et al., 2018). If the upper CS loses its ability to rotate, the middle and lower segments of the CS must attempt to make up for this restriction which predispose them to becoming hypermobile (having the ability to move past a normal range of movement) (Pop et al., 2018). This can result in an increased risk for spinal instability, degeneration, and pain (Pop et al., 2018). Other conditions associated with FHP include myofascial trigger points, anterior neck tightness/pain, temporomandibular joint (TMJ) disorders, rounded shoulders, as well as its promotion of respiratory inefficiency. Myofascial trigger points (MTP) are painful regions within a tight band of skeletal muscle and also give rise to referred pain (pain perceived at a different location than the source) (Simons et al., 1999). FHP results in increased load bearing on the musculature in the upper CS which can reduced pain thresholds as well as predispose MTP (Hong, 2019; Patwardhan et al., 2018). Overactive musculature and MTP's in the upper CS can predispose and contribute to the development of cervicogenic headaches (headaches originating from the neck) (Barmherzig & Kingston, 2019). The most common areas of the head that individuals experience a cervicogenic headache are the posterior and lateral aspects (Barmherzig & Kingston, 2019). A link also exists between FHP and TMJ function (Chaves et al., 2014; Zafar, et al., 2000). FHP contributes to the development of pain in the TMJ region by altering length-tension relationships in head and neck musculature (Chaves et al., 2014). FHP creates excessive tension in the muscles above the hyoid bone which, in turn, places greater force demands on the muscles that close the jaw (An et al., 2015). Over time, excessive force demands on the jaw muscles can lead to the development of myofascial trigger points and TMJ pain (Fernandez-de-las-Penas et al., 2010). This can contribute to the onset of anterior neck tightness or pain, as well as contribute to other symptoms such as difficulty swallowing food (An et al., 2015; Zheng, et al., 2012). Restoring postural alignment of the head and neck has been demonstrated to reduce myofascial symptoms by re-establishing normal hyoid bone position (Pettit & Auvenshine, 2018). Many individuals with FHP also demonstrate anterior rounding of the shoulders and upper back as well. As FHP is associated with overactivity of the upper trapezius and levator scapulae muscles. This condition can not only contribute to rounded shoulders, but negatively impact the normal movement patterns of the humerus and scapula (a condition known as scapular dyskinesis)(Bayattork et al., 2019). Rounding of the shoulders also predisposes the development of shoulder pain and impingement (Bayattork et al., 2019). The thoracic spine, especially the upper thoracic region, contributes to neck mobility (Tsang et al., 2013). Increased thoracic kyphosis (excessive anterior rounding of the upper back), can also promote hyperextension in the upper CS, which can lead to neck pain and stiffness (Roussouly, 2011). Additionally, a forward-held head, rounded shoulders, and excessive TK predisposes contracture (shortening) of the pectoral muscles, which also negatively affects overhead reaching ability (Olszewska, et al., 2018). If both FHP and rounding of the shoulders is occurring at the same time, this postural distortion is known as upper crossed syndrome (Janda, 2002). Another negative influence of sustained FHP is the promotion of respiratory inefficiency. Normal inspiration (breathing in) is initiated by contraction of the primary respiratory muscles- the diaphragm and external intercostal muscles (Kenney et al., 2015). However, in individuals with FHP, muscle activity and function of the diaphragm may decrease, which can reduce lung expansion during inspiration (Okuro et al., 2011). To make up for impaired muscle power of the diaphragm, individuals with FHP may compensate by utilizing accessory respiratory muscles such as the sternocleidomastoid (SCM) muscle to inspire air (Okuro et al., 2011). Excessive SCM activity when breathing at rest can cause an individual's shoulders and rib cage to move up and down rather than remaining in their normal stationary position (Okuro et al., 2011). Correction of FHP has been demonstrated to improve respiratory function and efficiency (Kim, et al., 2015). To help pass the time during the coronavirus pandemic, many individuals who have been confined at home have been engaging in excessive t.v. watching and extensive use of computers, tablets, and phones (Bowles, 2020). Individuals who maintain poor or awkward neck posture for prolonged periods of time during these activities are susceptible for neck pain and muscle strains. For example, using a laptop computer that is placed on one's legs results in greater neck flexion, torque and neck strain compared to using a standard computer that is located on a desk (Berkhout et al., 2004). In addition to neck pain, if poor posture is habitually sustained during these or other daily activities, it may also lead to muscle and spinal remodeling which can eventually result in permanent FHP (Dimitriadis, 2015). As video game playing can facilitate intense concentration and maintenance of awkward postures, children and young adults who play video games excessively may be at higher risk of developing musculoskeletal disorders (Gillespie, 2002). If FHP is not addressed and excessive gaming continues as they age, children will bring their skeletal malalignments into adulthood which puts them at higher risk for chronic postural abnormalities and spinal degenerative changes over their lifespan (Pop et al., 2018; Stone et al., 2015). While the invention of cell phones has enhanced our ability to rapidly communicate with each other, looking down at a phone for extended periods of time can accentuate FHP and contribute to the onset of neck pain (Damasceno et al., 2018; Gustafsson et al, 2017). Spinal surgeons have been reporting an increase in patients who are experiencing upper back and neck pain due to cell phone use (Cuellar & Lanman, 2017). A new diagnosis, known as "text neck", has been established to describe this condition (Cuellar & Lanman, 2017). The adult human head weighs approximately 10-12 pounds, however when the neck flexes to enable an individual to look down at a cell phone held in the hand, the relative stress placed on the neck increases significantly higher than just the weight of the head (Hansraj, 2014). Maintaining FHP for extended periods of time when working at your home or office can lead to pain in the CS as well as musculoskeletal symptoms in other body regions such as the shoulders, back, wrist, and hands (Borhany, et al., 2018). In addition, sitting with abnormal head and neck posture while working on a computer is also associated with higher incidences of headaches (Mingels et al., 2016). Having greater awareness of posture and utilizing a supportive and ergonomic office equipment can help reduce the occurrence of musculoskeletal disorders (Mani, et al., 2016). *Important: The specific treatment of pain is well outside a fitness professional's scope of practice. If your client is experiencing neck pain, it is important that the fitness professional stay within their scope of practice by referring them to a health care professional who is licensed to diagnose and treat their condition, and clear them for participating in fitness programs. Compensation Potential Overactive Muscles Potential Underactive Muscles Potential Related Injuries Forward head ● Sternocleidomastoid (SCM) ● Levator scapulae ● Scalenes ● Upper trapezius ● Suboccipitals ● Deep cervical flexors ● Cervical erector spinae ● Lower trapezius ● Rhomboids ● Headaches ● Dizziness ● Lightheadedness ● Shoulder pain ● Trapezius-levator scapulae dysfunction Self-myofascial release: Daily, 1 set, Hold tender spots for 30-90 seconds depending on intensity of application. * Important: There are several areas of the body to avoid using a foam roller for self-myofascial release due to risk of causing pain or potential injury in the structures below the skin. The CS is a great example of a contraindicated region for foam roller use due to the sensitive nature of this region of the body. To ensure client safety, it is also recommended that the fitness professional address inhibition of the sternocleidomastoid and suboccipitals utilizing the self-applied pressure technique rather than use of instrument-assisted devices. Foam roll the thoracic spine (Do not foam roll the cervical spine)* Perform instrument-assisted self-myofascial release for the levator scapulae and upper trapezius (Do not foam roll) Perform self-applied pressure to the SCM and suboccipitals Perform static stretching of shortened muscles: Daily, 1-4 repetitions, 20-30s hold. The supine chin tuck and curl exercise targets activation of the deep cervical flexors, which are commonly underactive in individuals with forward head posture. Step 1: instruct the client to perform a chin tuck (moving their chin straight back). Step 2: while maintaining the chin tuck position, instruct the client to contract their deep neck flexor muscles by attempting to lift their head off of the towel roll, however their head should not raise off the towel, rather they are performing an isometric contraction of the deep flexor muscles. Step 3: NASM recommendations for positional isometric exercises includes 1 set of 4 repetitions holding the isometric contraction for 4 seconds during each repetition with 2 second's rest between contractions. In step 2, client lifts their head 1 inch off towel roll, hold for 2 seconds, then lower head back to towel roll in 4 seconds time. Client performs 3-5 repetitions, with gradual progression to 10 repetitions as strength is gained. In step 2, client lifts their head 2-3 inches off towel roll, hold for 2 seconds, then lower head back to towel roll in 4 seconds time. Client performs 3-5 repetitions, with gradual progression to 10 repetitions as strength is gained. Important: The fitness professional should NOT apply any direct pressure to the client's head during this exercise. Chin Tuck The chin tuck exercise activates the cervical erector spinae (cervical extensors) which are commonly underactive in individuals with forward head posture. Step 1: Instruct the client to place two fingertips on their chin. Step 2: Instruct the client to apply light pressure in the posterior direction with their fingertips to help guide their head posteriorly to tuck their chin (and head) in this same direction moving out of forward head posture. Following the NASM isolated strengthening cadence, clients will isometrically hold their head in the tucked position for 2 seconds, and then return their head back to the starting position in 4 seconds time. Using NASM recommendations for isolated strengthening exercises, the client can perform 1-2 sets of 10-15 repetitions, 3-5 days per week. Note: Once the client understands how to perform this exercise correctly, this exercise can be performed without use of fingertips on the chin. After the client has been performing the chin tuck exercise below for at least 2 weeks, a chin tuck with band resistance can be implemented. The chin tuck with band resistance exercise activates and strengthens the cervical erector spinae (cervical extensors) which are commonly underactive in individuals with forward head posture. Step 1: Provide the client with an exercise band that is 4 to 5 feet in length. (Important. Begin with using a light resistance band and gradually progress to bands of heavier resistance). Step 2: With the client in a seated position, assist them to place the middle portion of the exercise band around the back of their head while holding on to the ends band with their hands in front of them at eye level. In this starting position, their shoulders and elbows should be flexed at a 90 degree angle (as shown in the image). Step 3: Instruct the client to perform a chin tuck against the resistance of the band, while at the same time extending their elbows (as shown in the second image). Following the NASM isolated strengthening cadence, clients will isometrically hold their head in the tucked position against band resistance for 2 seconds, and then return their head back to the starting position, while flexing their elbows back to a 90 degree angle in 4 seconds time. Using NASM recommendations for isolated strengthening exercises, the client can perform 1-2 sets of 10-15 repetitions, 3-5 days per week. The scapula retraction in prone exercise activates and strengthens the rhomboid muscles which are commonly underactive in individuals with rounded shoulders and forward head posture. Step 1: Client lies prone, face-down. The client's arms are relaxed by their side. Step 2: Instruct the client to "squeeze their shoulder blades together" while also raising their arms approximately 2 to 3 inches off of the floor. Following the NASM isolated strengthening cadence, clients will isometrically hold this position for 2 seconds, and then slowly return back to the starting position in 4 seconds time. Using NASM recommendations for isolated strengthening exercises, the client can perform 1-2 sets of 10-15 repetitions, 3-5 days per week. This first progression of the scapula retraction in prone exercise also activates and strengthens the rhomboid muscles which are commonly underactive in individuals with rounded shoulders and forward head posture. By modifying the arm position, it increases the difficulty of this exercise, as well as activation of the rhomboid musculature. Step 1: Client lies prone, face-down. The client's arms are resting on the floor in the following position: shoulders abducted (moved away from their side) to a 90 degree angle, elbows are flexed to a 90 degree angle. Step 2: Instruct the client to raise their arms approximately 2 to 3 inches off of the floor and "squeeze their shoulder blades together." Following the NASM isolated strengthening cadence, clients will isometrically hold this position for 2 seconds, and then slowly return back to the starting position in 4 seconds time. Using NASM recommendations for isolated strengthening exercises, the client can perform 1-2 sets of 10-15 repetitions, 3-5 days per week. This second progression of the scapula retraction in prone exercise also activates and strengthens the rhomboid muscles which are commonly underactive in individuals with rounded shoulders and forward head posture. By modifying the arm position further away from the body, it substantially increases the difficulty of this exercise to allow for greater activation of the rhomboids. Step 1: Client lies prone, face-down. The client's arms are resting on the floor in the following position: shoulders abducted (moved away from their side) to a 90 degree angle, elbows are extended (straight). Step 2: Instruct the client to raise their arms approximately 2 to 3 inches off of the floor while "squeezing their shoulder blades together." Following the NASM isolated strengthening cadence, clients will isometrically hold this position for 2 seconds, and then slowly return back to the starting position in 4 seconds time. Using NASM recommendations for isolated strengthening exercises, the client can perform 1-2 sets of 10-15 repetitions, 3-5 days per week. Step 1: Instruct your client to lie in a plank position on an exercise ball placed under the abdomen. The client's shoulders are abducted to 90 degrees with elbows extended and hands resting on the floor holding a light weight. Step 2: Instruct the client to first perform a chin tuck followed by moving their arms up toward the ceiling until they are horizontal to the floor. Between each repetition, the client should relax their head back to neutral position. Using NASM recommendations for integration exercises, the client can perform 1-3 sets of 10-15 repetitions (using a slow and controlled duration of repetition), 3-5 days per week. Step 1: The client holds light dumbbells in their hands. Instruct the client to descend into a squat using an exercise ball behind the thoracic spine. The client's arms should remain by their side with elbows extended during the descending phase. Step 2: Instruct the client to ascend back to the upright standing position while at the same time raising their arms upward in the scapular plane until their arms are parallel with the ground (this plane is located approximately 30-45 degrees anterior to the frontal plane - see photo). Using NASM recommendations for integration exercises, the client can perform 1-3 sets of 10-15 repetitions (using a slow and controlled duration of repetition), 3-5 days per week. Step 1: The client stands with feet side-by-side, shoulder width apart and places one hand on their hip. Step 2: The client holds to a cable handle with the opposite hand with shoulder flexed to 90 degrees and elbow extended. Step 3: The client descends into a squat position. Step 4: The client returns back to a standing position while at the same time performing one-arm row. After the set, the client repeats the above steps to integrate the opposite side of their body. Using NASM recommendations for integration exercises, the client can perform 1-3 sets of 10-15 repetitions (using a slow and controlled duration of repetition), 3-5 days per week. Step 1: Instruct the client to get into a split stance by placing one foot forward and place their hand on their hip. Step 2: The client holds to a cable handle with their OPPOSITE side hand, shoulder flexed to 90 degrees and elbow extended. (for example, if the left foot is forward, the client uses their right hand to row). Step 3: The client performs a single-arm row while at the same time rotating their trunk approximately 90 degrees toward the side of their body that is performing the row. Step 4: The client returns back to step 2 position. After the set, the client repeats the above steps to integrate the opposite side of their body. Using NASM recommendations for integration exercises, the client can perform 1-3 sets of 10-15 repetitions (using a slow and controlled duration of repetition), 3-5 days per week. The more aware we are of the problems and solutions with tech neck in ourselves, the better we can support our clients. Take time to practice the NASM Corrective Exercise Continuum on yourself using self-myofascial release, static stretching, focused strengthening exercises and integrated dynamic movements. Below are examples from each stage of the continuum. Once you feel confident in the approach, apply the model to your clients. Muscles targeted: Upper trapezius, levator scapulae, sternocleidomastoid (SCM). Add corrective strategies to the mix by using self-myofascial release (i.e., teach clients how to do this). Target the upper trapezius and levator scapulae with a small ball or tools like a Backnobber® (backnobber-store.com) or Thera Cane® (theracane.com). Find tender spots along these muscles and hold pressure against each spot until the tenderness has subsided (30–60 seconds). STATIC STRETCHING Because sensitive nerves and blood vessels are located in the neck near the SCM, use static stretches for this area (SCM, scalenes, levator scapulae) instead of SMR. Hold for 30 seconds. QUADRUPED While on all fours, let the head drop toward the floor in the forward-head position. Then retract the head into a neutral position, drawing a straight line from ears to shoulders to hips. The quadruped position allows the exercise to be done directly against gravity, providing a bit more resistance than is possible in the standing position. Do 10–15 reps with a 2-second isometric hold. Note: This exercise does not call for heavy resistance to weigh down the head and "muscle it" out of the tech-neck form. To train the nervous system to encode a new pattern, frequent repetition of lightly resisted movements is all that is needed. Do not let the simplicity of the exercise lead you to think it does not work. This is a very effective exercise that clients can perform easily without equipment. PUSHUP INTEGRATION Integration exercises are often full-body moves that place a particular focus on the area being addressed. Pushups are a good choice here, as they put the head and neck in the same position as the activation exercise listed above, but with added work. It is important to cue clients to focus more on the head and neck position and less on how many pushups they can do. Modify the exercise to meet each client's needs. Aim for 10–15 reps. An, J. S., Jeon, D. M., Jung, W. S., Yang, I. H., Lim, W. H., & Ahn, S. J. (2015). Influence of temporomandibular joint disc displacement on craniocervical posture and hyoid bone position. American Journal of Orthodontics and Dentofacial Orthopedics, 147(1), 72-79. doi:10.1016/j.ajodo.2014.09.015 Bayattork, M., Seidi, F., Minoonejad, H., McClure, P., & Mozafaripoor, E. (2019). Intra-rater and inter-rater reliability and agreement of the scapular dyskineis test in young men with forward head and round shoulder posture. Journal of Rehabilitation Sciences and Research, 6(4), 169-173. Barmherzig, R., & Kingston, W. (2019). Occipital neuralgia and cervicogenic headache: Diagnosis and management. Current Neurology and Neuroscience Reports, 19(5), 20. doi:10.1007/s11910-019-0937-8 Berkhout, A. L., Hendriksson-Larsen, K., & Bongers, P. (2004). The effect of using a laptop station compared to using a standard laptop PC on the cervical spine torque, perceived strain and productivity. Applied Ergonomics, 35(2), 147-152. doi:10.1016/j.apergo.2003.11.008 Borhany, T., Shahid, E., Siddique, W. A., & Ali, H. (2018). Musculoskeletal problems in frequent computer and internet users. Journal of Family Medicine and Primary Care, 7(2), 337-339. doi:10.4103/jfmpc.jfmpc_326_17 Bowles, N. (2020, March 31). Coronavirus ended the screen-time debate. Screens won. The New York Times.https://www.nytimes.com/2020/03/31/technology/coronavirus-screen-time.html Cuellar, J.M. & Lanman, T.H. (2017). "Text neck": an epidemic of the modern era of cell phones? The Spine Journal, 17, 901-902. Chaves, T. C., Turci, A. M., Pinheiro, C. F., Sousa, L. M., & Grossi, D. B. (2014). Static body postural misalignment in individuals with temporomandibular disorders: a systematic review. Brazilian Journal of Physical Therapy, 18(6), 481-501. doi:10.1590/bjpt-rbf.2014.0061 Clark, M. A., Lucett, S. C., & Sutton, B. G. (2014). NASM Essentials of Corrective Exercise Training, 1st ed. revised. Jones & Bartlett Learning. Damasceno, G. M., Ferreira, A. S., Nogueira, L. A. C., Reis, F. J. J., Lara, R. W., & Meziat-Filho, N. (2018). Reliability of two pragmatic tools for assessing text neck. Journal of Bodywork and Movement Therapies, 22(4), 963-967. doi:10.1016/j.jbmt.2018.01.007 Dimitriadis, Z., Podogyros, G., Polyviou, D., Tasopoulos, I., & Passa, K. (2015). The reliability of lateral photography for the assessment of the forward head posture through four different angle-based analysis methods in healthy individuals. Musculoskeletal Care, 13(3), 179-186. Fernandez-de-las-Penas, C., Galan-del-Rio, F., Alonso-Blanco, C., Jimenez-Garcia, R., Arendt-Nielsen, L., & Svensson, P. (2010). Referred pain from muscle trigger points in the masticatory and neck-shoulder musculature in women with temporomandibular disorders. The Journal of Pain, 11(12), 1295-1304. Gillespie, R. M. (2002). The physical impact of computers and electronic game use on children and adolescents, a review of current literature. Work, 18(3), 249-259. Gustafsson, E., Thomee, S., Grimby-Ekman, A., & Hagberg, M. (2017). Texting on mobile phones and musculoskeletal disorders in young adults: A five-year cohort study. Applied Ergonomics, 58, 208-214. doi:10.1016/j.apergo.2016.06.012 Hansraj, K. K. (2014). Assessment of stresses in the cervical spine caused by posture and position of the head. Surgical Technology International, 25, 277-279. Hong, S. W., Lee, J. K., & Kang, J. H. (2019). Relationship among cervical spine degeneration, head and neck postures, and myofascial pain in masticatory and cervical muscles in elderly with temporomandibular disorder. Arch Gerontol Geriatr, 81, 119-128. doi:10.1016/j.archger.2018.12.004 Janda, V. (2002). Muscles and motor control in cerviogenic disorders. In: Grant, R. ed. Physical Therapy of the Cervical and Thoracic Spine. Churchill Livingstone. Kenney, W., Wilmore, J., Costill, D. (2015). Physiology of Sport and Exercise, 6th Ed. Human Kinetics. Kim, S.Y., Kim, N.S., Kim, L.J. (2015). Effects of cervical sustained natural apophyseal glide on forward head posture and respiratory function. Journal of Physical Therapy Science, 27, 1851-1854. Mani, K., Provident, I., & Eckel, E. (2016). Evidence-based ergonomics education: Promoting risk factor awareness among office computer workers. Work, 55(4), 913-922. doi:10.3233/WOR-162457 Mingels, S., Dankaerts, W., van Etten, L., Thijs, H., & Granitzer, M. (2016). Comparative analysis of head-tilt and forward head position during laptop use between females with postural induced headache and healthy controls. Journal of Bodywork and Movement Therapies, 20(3), 533-541. doi:10.1016/j.jbmt.2015.11.015 Okuro, R. T., Morcillo, A. M., Ribeiro, M. A., Sakano, E., Conti, P. B., & Ribeiro, J. D. (2011). Mouth breathing and forward head posture: effects on respiratory biomechanics and exercise capacity in children. Brazilian Journal of Pulmonology, 37(4), 471-479. doi:10.1590/s1806-37132011000400009 Olszewska, E., Tabor, P., & Czarniecka, R. (2018). Magnitude of physiological curvatures of the spine and the incidence of contractures of selected muscle groups in students. Biomedical Human Kinetics, 10, 31-37. Patwardhan, A. G., Khayatzadeh, S., Havey, R. M., Voronov, L. I., Smith, Z. A., Kalmanson, O., . . . Sears, W. (2018). Cervical sagittal balance: a biomechanical perspective can help clinical practice. European Spine Journal, 27(Suppl 1), 25-38. doi:10.1007/s00586-017-5367-1 Pettit, N. J. & Auvenshine, R. C. (2018). Change of hyoid bone position in patients treated for and resolved of myofascial pain. Cranio, 31, 1-17. Pop, M.S., Mihancea, P., & Debucean, D. (2018). Posture optimization- Is it the key to myofascial neck pain relief? Archives of the Balkan Medical Union, 53(4), 573-579. Roussouly, P., & Pinheiro-Franco, J. L. (2011). Sagittal parameters of the spine: biomechanical approach. European Spine Journal, 20 Suppl 5, 578-585. doi:10.1007/s00586-011-1924-1 Simons, D. G., Travell, J. G., Simons, L. S. (1999). Travell & Simons' myofascial pain and dysfunction: Upper half of body. Lippincott Williams & Wilkins. Stone, M. A., Osei-Bordom, D. C., Inman, R. D., Sammon, C., Wolber, L. E., & Williams, F. M. (2015). Heritability of spinal curvature and its relationship to disc degeneration and bone mineral density in female adult twins. European Spine Journal, 24(11), 2387-2394. doi:10.1007/s00586-014-3477-6 Tsang, S., Szeto, G., & Lee, R. (2013). Normal kinematics of the neck: The interplay between cervical and thoracic spines. Manual Therapy, 18(5), 431-437. Zafar, H., Nordh, E., & Eriksson, P. O. (2000). Temporal coordination between mandibular and head-neck movements during jaw opening-closing tasks in man. Archives of Oral Biology, 45(8), 675-682. Zheng, L., Jahn, J., & Vasavada, A. N. (2012). Sagittal plane kinematics of the adult hyoid bone. Journal of Biomechanics, 45(3), 531-536. doi:10.1016/j.jbiomech.2011.11.040What is Forward Head Posture (FHP)?
Five Negative Impacts of Forward head posture

#1 Myofascial Trigger Points and Headaches:
#2 Temporomandibular joint (TMJ) disorders:
#3 Anterior Neck Tightness/Pain
 FHP also increases tension in the musculature located directly above the hyoid bone (a small bone located in the upper neck below the jaw) which can cause this bone to elevate above its normal resting position. (Zheng, et al., 2012).
FHP also increases tension in the musculature located directly above the hyoid bone (a small bone located in the upper neck below the jaw) which can cause this bone to elevate above its normal resting position. (Zheng, et al., 2012). #4 Rounded Shoulders and Upper Back
#5 Respiratory Inefficiency
Maintaining Poor Posture during Excessive Screen-Time
Maintaining Poor Posture during Excessive Gaming
 Not only are adults susceptible for FHP development, but children and adolescents are also at risk. Video game use among children and adolescents has risen substantially over the last decade.
Not only are adults susceptible for FHP development, but children and adolescents are also at risk. Video game use among children and adolescents has risen substantially over the last decade. Maintaining Poor Posture when Texting - "Text Neck"
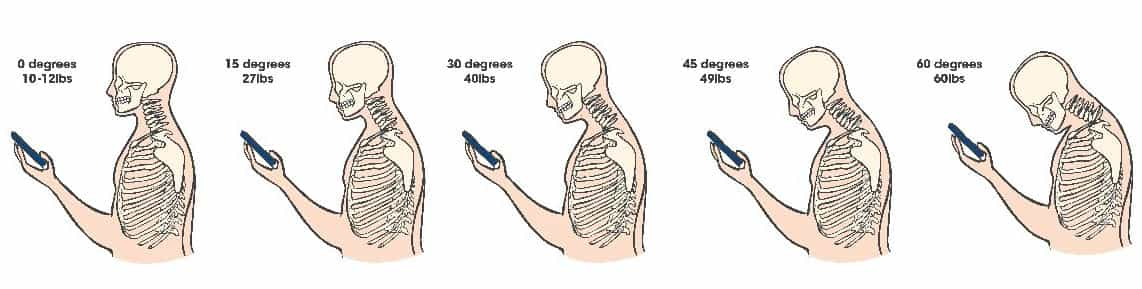
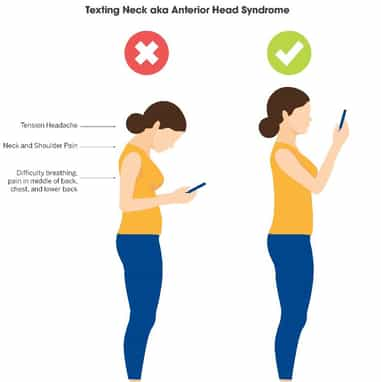 When the neck is flexed to 15 degrees, the relative stress on the neck can increased to approximately 30 pounds, 30 degrees of neck flexion can increase the relative stress to 40 pounds, 45 degrees can increase the relative stress to 50 pounds, and 60 degrees of neck flexion increases the relative neck stress to 60 pounds (Hansraj, 2014). Using recommended posture when texting on cell phones can help prevent the onset of "text neck."
When the neck is flexed to 15 degrees, the relative stress on the neck can increased to approximately 30 pounds, 30 degrees of neck flexion can increase the relative stress to 40 pounds, 45 degrees can increase the relative stress to 50 pounds, and 60 degrees of neck flexion increases the relative neck stress to 60 pounds (Hansraj, 2014). Using recommended posture when texting on cell phones can help prevent the onset of "text neck." Maintaining Poor Posture Working on the Computer
Using the Corrective Exercise Continuum to Improve Forward head posture
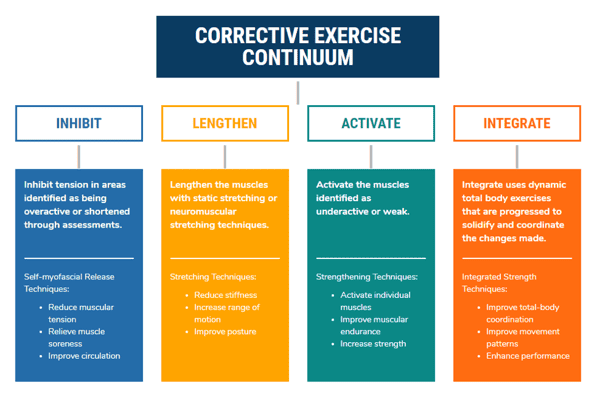 By using corrective exercise techniques to address postural and movement dysfunctions, it can help prevent the negative impacts of FHP. Follow the steps of NASM's Corrective Exercise Continuum below.
By using corrective exercise techniques to address postural and movement dysfunctions, it can help prevent the negative impacts of FHP. Follow the steps of NASM's Corrective Exercise Continuum below.
Step 1: Inhibit overactive muscles

Step 2: Lengthen shortened muscles



Step 3: Activate underactive muscles
Supine Chin Tuck and curl
Beginner:
Intermediate
Advanced
Progression - Chin tuck with band
Scapula Retraction in Prone


Progression 1
Progression 2
Step 4: Integrate dynamic movement patterns

Ball combo with chin tuck - T Position
Ball Squat to Scaption
Squat to Row
Single-Arm Row to Arrow Position Start and Finish
Additional Corrective Strategies for Tech Neck

Inhibit: Self-Myofascial Release

Lengthen: Static Stretching

Activate: Strengthening Exercise

Integrate: Solidify and Coordinate
For more relevant resources check these blog posts out!
References:
How To Fix Full Body Posture
Source: https://blog.nasm.org/fixing-forward-head-posture
Posted by: greenvory1971.blogspot.com

0 Response to "How To Fix Full Body Posture"
Post a Comment